Fatty liver disease quietly builds excess fat in the liver, often without early warning signs, turning a vital organ into a risk for serious issues. Affecting about 25% of people worldwide, it links closely to obesity, diabetes, and poor diet—trends health experts at Sound Health and Lasting Wealth and CDC track as rising sharply. Medical professionals stress early awareness and changes, as research shows reversal is possible in initial stages before scarring sets in.
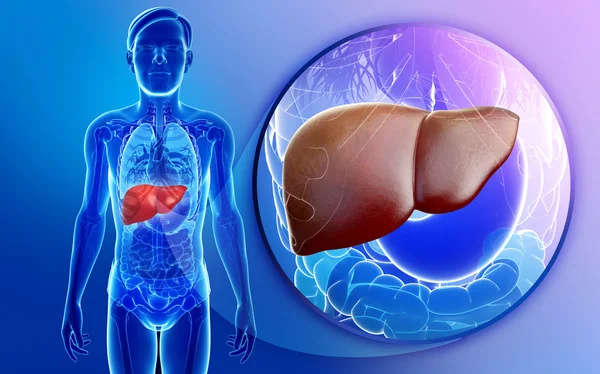
What Is Fatty Liver Disease?
Fatty liver disease, now often called metabolic dysfunction-associated steatotic liver disease (MASLD), happens when fat makes up more than 5% of liver cells, unrelated to heavy alcohol in most cases. Two main types exist: MASLD from metabolic factors like high blood sugar, and alcohol-related liver disease from excess drinking. According to health experts, MASLD has surged to impact 1 in 3 adults, driven by obesity rates climbing globally.
This buildup starts harmless but can progress to inflammation (MASH), fibrosis, cirrhosis, or even liver cancer if unchecked. Projections indicate prevalence could hit 55.7% by 2040 without interventions, a three-fold rise since 1990. Early detection through blood tests or ultrasounds helps halt advancement, as the liver holds strong regenerative power when supported.
Common Symptoms to Watch
Many with fatty liver notice no symptoms until damage advances, making routine checks vital for at-risk groups. Fatigue and weakness top the list, often dismissed as aging or stress, alongside vague upper right abdominal discomfort. Weight loss or loss of appetite may appear later, with advanced cases showing itchy skin, leg swelling, or jaundice—yellowing of eyes and skin.
Research suggests these signs overlap with diabetes or heart issues, complicating self-diagnosis. Pain or fullness under the ribs signals inflammation for some, while enlarged spleen or easy bruising hints at fibrosis. Medical professionals recommend tracking patterns, especially if metabolic syndrome factors like high cholesterol cluster. Seek evaluation for blood in stool or breathing trouble, as these raise red flags.
Key Causes and Risk Factors
Obesity drives most MASLD cases, with excess body fat—particularly around the waist—pushing lipids into liver cells. Type 2 diabetes and insulin resistance follow closely, as high blood sugar disrupts fat metabolism, per CDC insights. High cholesterol, hypertension, and metabolic syndrome amplify risks, affecting up to 38.9% globally in 2020.
Other contributors include rapid weight loss, certain medications like corticosteroids, or viruses such as hepatitis C. Genetics play a role, but lifestyle dominates—sedentary habits and sugary diets tip the balance. For alcohol-related types, moderate to heavy intake over years overloads the liver directly. Smokers face steeper odds, with studies showing faster progression.
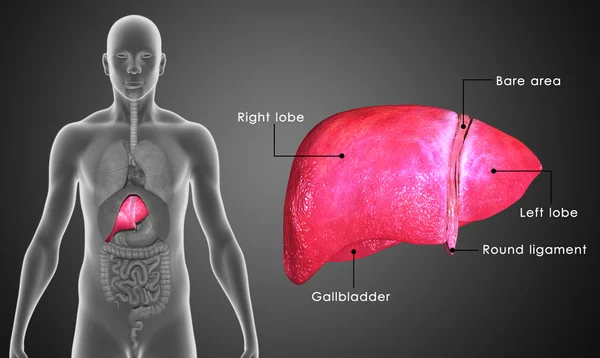
Diagnosis Methods Explained
Doctors start with blood tests checking liver enzymes like ALT and AST, which rise with fat buildup or inflammation. Ultrasound often spots fatty changes as a bright liver echo, quick and non-invasive. FibroScan measures stiffness for fibrosis without biopsy in many cases.
Advanced imaging like MRI or CT confirms severity, while biopsy—removing a small tissue sample—provides definitive staging for MASH or cirrhosis. Health experts at Mayo Clinic note risk calculators like FIB-4 score help prioritize screenings for those over 50 or with diabetes. Regular monitoring catches issues early, guiding precise management.
Proven Prevention Strategies
Lifestyle shifts form the core defense, with weight loss of 5-10% reversing fat in early MASLD per clinical data. A Mediterranean-style diet rich in fruits, vegetables, whole grains, nuts, and fish cuts red meat and sugars, slashing steatosis risk. Aim for 150 minutes weekly of moderate exercise like brisk walking to boost fat burning.
Limit alcohol to under one drink daily for women and two for men; vaccinate against hepatitis A/B to protect the liver. Control blood sugar and cholesterol through balanced meals—plate half veggies, quarter protein, quarter grains. Public health guidelines from WHO emphasize these steps blunt genetic risks too. Track progress with your doctor every 6-12 months.
Treatment Options Overview
No single pill cures fatty liver, but managing root causes halts progression effectively. Weight loss via diet and exercise tops recommendations, with studies showing 7-10% reduction easing inflammation. Doctors may prescribe meds for diabetes or cholesterol if needed, like statins safe for mild cases.
Vitamin E shows promise for non-diabetics without cirrhosis, reducing fat and swelling, though more trials continue. Omega-3s from fish oil aid some, but only under guidance. Advanced MASH might need specialists for fibrosis drugs in trials. Always pair with habits; shorter alcohol abstinence aids recovery in ALD.
FAQ
What are the first signs of fatty liver disease?
Fatigue, right-side belly pain, and weakness often emerge first, though many stay symptom-free until later stages. Blood tests reveal elevated enzymes early.
Can fatty liver be reversed naturally?
Yes, research suggests 5-10% weight loss through diet and exercise reverses early MASLD in most cases. Consistency matters over quick fixes.
Is fatty liver linked to diabetes?
Strongly—insulin resistance from diabetes promotes fat buildup, with 70% of type 2 patients affected. Controlling sugar helps both.
Does alcohol cause all fatty liver?
No, MASLD stems from metabolism, not alcohol; heavy drinking causes a separate type. Both benefit from abstinence.
How common is fatty liver disease?
About 25-39% worldwide, rising with obesity; projections hit 55% by 2040 without changes.
Final Note
Fatty liver disease demands attention through sustainable habits that safeguard liver health long-term. Start with small steps like daily walks and veggie-focused meals, monitoring with annual checkups. Consult healthcare professionals for tailored plans, as early action preserves function and prevents complications.
Also Read | How to Get Better Sleep After 50: 7 Simple Tips for Pain‑Free Nights