Gut microbiota has emerged as a significant factor in Alzheimer’s disease (AD) research and therapy. The role of gut microbiota in AD pathogenesis has been increasingly recognized, leading to the exploration of various gut microbiome-targeted therapies. These include probiotics, prebiotics, synbiotics, postbiotics, and fecal microbiota transplantation (FMT), which have shown promise in the treatment and management of AD.
Alzheimer’s disease (AD) is a complex neurodegenerative disorder with no cure, making the gut microbiome a promising new area of research for potential therapeutic interventions.
This review explores the current understanding of the gut microbiome’s role in AD, potential microbiota-based therapies, and future research directions.
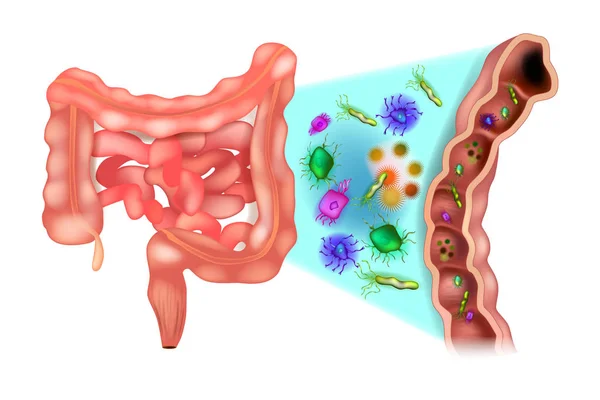
Recently, the gut microbiome, the diverse community of microbes residing in our gut, has emerged as a potential player in AD. Studies suggest a link between its composition and AD progression, opening doors for novel therapeutic strategies.
The Gut-Brain Connection
Direct invasion? Some propose gut microbes might directly infect the central nervous system (CNS), contributing to Aβ plaque buildup.
Indirect whispers: Others highlight the role of gut-brain communication through the vagus nerve and metabolites like short-chain fatty acids (SCFAs). These can influence brain inflammation, immunity, and energy production, potentially impacting AD pathology.
Microbial diversity decline: Studies show a decrease in gut microbiome diversity in AD patients compared to healthy individuals. Specific bacterial groups may be associated with disease progression.
Genetic influence: The APOE gene, a risk factor for AD, seems to influence the gut microbiome composition, adding another layer of complexity.
Therapeutic Hope
The burgeoning understanding of the gut-brain axis opens doors for exciting therapeutic possibilities. Here are some promising avenues currently being explored:
Antibiotics: While not a definitive cure, studies hint that past antibiotic use might be associated with a lower risk of dementia. However, further research is needed to understand the mechanisms and potential side effects.
FMT (Fecal Microbiota Transplantation): Replacing gut microbes with healthy ones through FMT has shown promise in reducing Aβ plaques and improving cognitive function in AD animal models and some human cases. This personalized approach holds immense potential for the future of AD treatment.
Probiotics and prebiotics: These dietary supplements and fibers may promote the growth of beneficial gut bacteria, potentially offering neuroprotective effects. While more research is needed to determine their specific benefits and optimal dosages, they represent a promising non-invasive strategy.
Challenges and Future Directions
Individuality: Gut microbiome composition varies greatly between individuals. Standardized methodologies and larger studies are needed to identify specific microbial signatures associated with AD and develop personalized treatment approaches.
Beyond bacteria: Fungi, viruses, and other gut microbes deserve further investigation for their potential role in AD.
Functional understanding: Studying the functional activities of gut microbes beyond their mere presence is crucial to understand their true impact on AD.
What are some challenges in developing gut microbiota-targeted therapies for alzheimer’s disease
Some of the challenges in developing gut microbiota-targeted therapies for Alzheimer’s disease (AD) include:
Complexity of the Microbiota-Gut-Brain Axis: The bidirectional communication between the gut and the brain, known as the microbiota-gut-brain axis, is complex, involving various physiological systems and pathways. Identifying specific pathways within this axis that are relevant to AD remains challenging.
Diversity of Microbiota: The diversity of gut microbiota among individuals makes it difficult to establish universal microbiota-targeted therapies. Personalized approaches may be necessary to account for this diversity.
Understanding Mechanisms: While there is evidence of the influence of gut microbiota on AD pathologies, such as Aβ accumulation, tau pathology, and neuroinflammation, the specific mechanisms involved are not fully understood.
Clinical Translation: Moving from preclinical research to clinical application of gut microbiota-targeted therapies poses challenges in terms of safety, efficacy, and standardization of interventions.
Host Factors: The impact of host factors, such as genetics, sex, and overall health, on the relationship between gut microbiota and AD adds another layer of complexity to the development of targeted therapies.
Conclusion
The gut microbiome is a fascinating and complex ecosystem with potential implications for AD. While much remains to be unraveled, ongoing research holds promise for developing novel therapeutic strategies targeting the gut-brain axis. By understanding the intricate interplay between gut microbes and AD, we may one day find a way to prevent or slow down this devastating disease. [ Source 1]
ALSO READ: Adolescent Obesity Linked To Early Chronic Kidney Disease In Young Adulthood