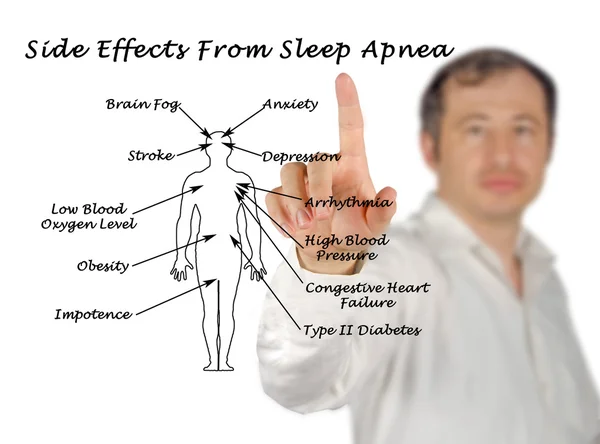
Sleep apnea is a serious sleep disorder characterized by repeated interruptions in breathing during sleep. It can lead to various health complications, including cardiovascular issues and daytime fatigue. Recent discussions among healthcare professionals have shed light on the genetic components of sleep apnea, particularly how conditions like menopause and polycystic ovary syndrome (PCOS) may elevate risk levels. This article explores the genetic and non-genetic risk factors associated with sleep apnea, as well as actionable strategies to mitigate its symptoms.

Are Genetics the Main Risk Factors of Sleep Apnea?
Research indicates that genetics play a significant role in the development of obstructive sleep apnea (OSA). Approximately 40% of the variance in OSA can be attributed to genetic factors. This heritability suggests that individuals with a family history of sleep apnea are more likely to develop the condition themselves. Key genetic risk factors include:
- Family History: A higher prevalence of OSA is observed among individuals with relatives who have been diagnosed with the disorder. Studies show that first-degree relatives of those with OSA often exhibit similar symptoms, such as snoring and observed apneas.
- Craniofacial Structure: Genetic predispositions affecting craniofacial anatomy can influence airway size and shape, which are critical in determining susceptibility to airway obstruction during sleep.
- Obesity: While obesity is a well-known risk factor for OSA, it also has genetic underpinnings. Certain genes may predispose individuals to obesity, thereby indirectly increasing their risk of developing sleep apnea.
- Neurological Control: Genetic variations affecting the neurological control of upper airway muscles can impact breathing patterns during sleep, contributing to OSA severity.
Despite these insights, much about the specific genes involved remains unclear, indicating a need for further research in this area.
Non-Genetic Risk Factors for Sleep Apnea
In addition to genetic influences, several non-genetic factors contribute significantly to the risk of developing sleep apnea:
- Obesity: Excess body weight is one of the most significant risk factors for OSA. Fat deposits around the neck can obstruct the airway during sleep.
- Age: The likelihood of developing sleep apnea increases with age due to changes in muscle tone and respiratory function.
- Gender: Men are more likely than women to develop OSA, although post-menopausal women see an increased risk due to hormonal changes.
- Menopause: The hormonal fluctuations during menopause can lead to weight gain and changes in body fat distribution, both of which elevate the risk for OSA.
- PCOS: Women with polycystic ovary syndrome often experience insulin resistance and obesity, both of which are linked to a higher incidence of sleep apnea.
- Lifestyle Choices: Smoking, alcohol consumption, and sedative use can relax throat muscles and exacerbate airway obstruction during sleep.
Awareness of these factors is crucial for early identification and intervention.
What You Can Do to Reduce Symptoms of Sleep Apnea
Managing sleep apnea often requires a multifaceted approach that includes lifestyle modifications and medical interventions. Here are some effective strategies:
- Weight Management: Losing even a small amount of weight can significantly reduce the severity of sleep apnea symptoms. Weight loss helps decrease fat deposits around the neck and improve airflow during sleep.
- Regular Exercise: Engaging in physical activity can enhance overall health and reduce symptoms. Aerobic exercises, resistance training, and yoga are particularly beneficial for strengthening airway muscles.
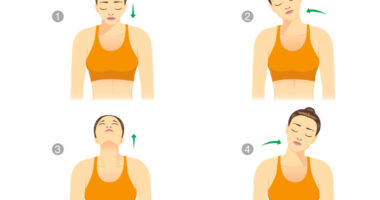
- Sleep Positioning: Sleeping on your side rather than your back can help keep your airway open. Side-sleeping prevents the tongue and soft tissues from collapsing into the throat.
- Elevate Your Head: Raising the head of your bed by four to six inches or using specialized pillows can help maintain an open airway during sleep.
- Avoid Alcohol and Sedatives: These substances relax throat muscles and can worsen sleep apnea symptoms. Limiting their intake—especially before bedtime—can be beneficial.
- Quit Smoking: Smoking contributes to inflammation and fluid retention in the upper airway, exacerbating sleep apnea symptoms.
- Use CPAP Therapy: Continuous positive airway pressure (CPAP) therapy is one of the most effective treatments for moderate to severe OSA. It involves wearing a mask connected to a machine that provides a steady stream of air to keep airways open during sleep.
By implementing these strategies, individuals can effectively manage their symptoms and improve their quality of life.

Conclusion
Understanding both genetic and non-genetic risk factors for sleep apnea is vital for effective management. As research continues to evolve, awareness about how conditions like menopause and PCOS affect susceptibility will help inform treatment approaches. Through lifestyle modifications and appropriate medical interventions, individuals at risk can take proactive steps toward better sleep health.
Also Read | Healthiest Sleeping Position: Back, Side, Or Stomach?