Almost every day, new findings on medical research are published, some of which may include complementary health approaches.
Research studies about medical treatments and practices published in scientific journals are often the sources of news stories and can be important tools in helping you manage your health.

But finding scientific journal articles, understanding the studies they describe, and interpreting the results can be challenging.
One way to make it easier to understand information you find in a scientific journal is to share the information with your health care providers and get their opinions. Once you understand the basics and terminology of scientific research, you have one more tool to help you make better, informed decisions about your health.
1. What are the parts of a scientific paper?
Most articles in scientific journals have a similar basic structure or format. There are five important parts of a research paper, which most articles contain.
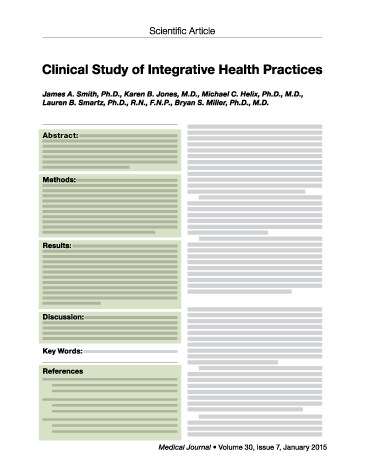
Example of a scientific journal article
Click on one of the highlighted areas to learn more
Abstract. A brief summary of the key points of the scientific paper.
Methods. Detailed information on how the study was performed.
Results. What the study showed. This section doesn’t attempt to evaluate the meaning of the results. It just presents the data, summaries, and analyses of the data collected from the study. Also, this section often includes tables, graphs, and charts that show the results.
Discussion and Conclusion. What the results mean. This is where you can often find out how the study relates to your own health. This section often includes the authors’ explanation of, and own opinions about, what the results mean. Since the conclusions are the authors’ own, others may or may not completely agree with their explanations of the results.
References. Previously published articles the authors used to review what related research was done before, to help design the study and interpret its results.
2. What were the goals of the study?
Basic research aims to understand fundamental biological processes, or the mechanisms by which a treatment might affect the body.
Translational research aims to create the “building blocks” of information necessary for rigorous investigation of the effects and safety of an intervention in human clinical trials. Both basic and translational research may employ studies done in the laboratory, or with volunteers in a clinical setting.
Clinical trials aim at testing whether an intervention is useful and safe in humans. They may vary in size and type.
- Preliminary, exploratory, or pilot studies provide essential stepping stones of information about the potential safety and usefulness of an intervention, and help scientists determine whether to perform larger, more definitive clinical trials.
- Well-planned clinical trials give the clearest information about whether a treatment or a lifestyle change is effective and safe. However, because they’re complicated, lengthy, and very, very expensive, they’re usually done only after smaller preliminary studies have been completed and have shown some promise that the treatment may be helpful to patients.
While all studies, from basic to translational to clinical, are extremely important, clinical trials (because they are done in people) are the types of studies you probably hear about most often in the news and can have the most immediate impact on improving health and treating disease. Therefore, the remaining questions focus on clinical trials.
3. How large was the study?
Studies with large numbers of people generally get results that are more reliable than studies with small pools of participants. Larger studies can increase the accuracy of the study findings and reduce the probability that any effect observed in the study was due to chance. Too few participants may make the entire study a failure—it may only produce inconclusive results. Statisticians and scientists have tools to figure out how many volunteers are needed for a clinical study to be meaningful.
Study tests new treatment in 50 people
People receiving the treatment feel much better, but the researchers may not be sure other people will benefit
Statistical tests can’t tell whether this effect is real or due to chance
Study tests new treatment in 500 people
People receiving the treatment feel much better
Statistical tests indicate that the effect is real
In general, a large study with many volunteers may be able to produce conclusive results when a small study may not.
4. Was the study a controlled clinical trial?
In a controlled clinical trial, investigators compare the effects of different treatments in groups of study participants who are as identical as possible in all other respects. For example, the outcomes in one group of participants who receive a new “experimental” treatment may be compared with the results of another group who received standard care, the “control group.” In effect the control group provides a “yardstick” for measuring the effects of the new treatment. In this case standard care is the “control” intervention.
Experimental group
Participants receive new treatment
Participants are observed, and results are recorded
Control group
Participants receive standard care
Participants are observed, and results are recorded
Design of a clinical trial in which a new treatment is compared to standard care.
What did the control group receive?
There are many kinds of control groups. Ideally, participants are assigned randomly to one of the study groups. This helps ensure that the two groups are as identical in all respects as possible except for the intervention they receive. Other kinds of control groups are sometimes used, but they have an increased likelihood that factors other than the intervention affected the results.
In placebo-controlled trials, the control group receives an inactive treatment designed to resemble the treatment being studied. One example of a placebo is a pill that is medically inert (inactive) but looks like the experimental medicine being studied. Another example, called a sham, is used when the treatment being studied is a procedure (e.g., acupuncture), not a product. A sham procedure is designed to simulate the active treatment but does not have any active treatment qualities. When possible, the “placebo” treatment and “experimental” active treatment are delivered in a “double-blind” fashion. That is, neither the investigator delivering the treatment nor the volunteer know what they are getting. This reduces the possibility the volunteers know what they are receiving.
Experimental group
Participants receive the actual treatment
Participants and investigators don’t know which group each participant is in
Participants are observed, and results are recorded.
Control group
Participants receive an inactive (placebo or sham) treatment
Participants and investigators don’t know which group each participant is in
Participants are observed, and results are recorded.
Design of a clinical trial using a placebo or sham treatment
5. Have steps been taken to minimize bias?
It can be surprisingly difficult to avoid bias in clinical trials. For example, if patients know what treatment they received or if the investigators know which treatment a patient received, it may affect their impression of whether the patient improved–no matter how hard they try to avoid it. Therefore, it’s important to ask what steps were taken to minimize bias. For example, was the trial “blinded” or “masked” so that neither the participants nor the investigators knew who was receiving which treatment? Researchers must always work to make sure that the study is objective and the results reflect the data accurately.
6. Are there potential conflicts of interest?
In viewing the results of any study it is important to look for potential conflicts of interest or other sources of bias. It is useful to understand who funded the study. How removed were the sponsor and the investigators from any financial or reputational “stake” in the study outcome? Is there similar evidence from other independent sources? Fortunately, most medical journal articles now include information about relevant financial relationships.
7. How do the reported results compare with previous studies?
The strongest evidence about whether an intervention is useful and safe consists of results from several studies by different investigators. Rarely does a single study provide a final, definitive answer. There is a need for a study to be replicated, which involves repeating a study using the same methods but with different volunteers and investigators. Replication of a study gives more confidence that the results are reliable and valid. In addition, independent evaluations that compile the results of multiple studies and rigorously assess the quality of the data from them are especially useful. These evaluations are called systematic reviews and meta-analyses.
8. What does it mean when the results of a study are described as statistically significant but not clinically significant?
“Statistically significant” means the finding in the difference between the study groups is not likely to be due to chance. “Clinically significant” is a measure of the size of the effects observed in the study. For example, a study can find statistically significant differences between two treatment groups, but the differences are so small that they do not have clinical significance in terms of usefulness for patients or safety.
9. How old is the study?
Look at the date of the study. Was it conducted in the last few years? Have there been more recent studies? You can search the National Library of Medicine’s PubMed for published studies.
Sometimes, new research can dramatically change scientists’ view of a topic. For example, older pilot studies may have suggested that a particular complementary approach may be helpful for a certain medical problem, but a new, large clinical trial might show that it doesn’t have beneficial effects. The GEM study, on Ginkgo biloba for dementia, is one example. This study was the largest clinical trial ever to evaluate ginkgo’s effect on the occurrence of dementia, and although the results failed to show benefit of ginkgo in preventing dementia in older adults, the study confirmed the importance of randomized trials in determining the therapeutic benefit for complementary therapies. From a research point of view, the study also provided researchers with important information about how to design and conduct large dementia prevention trials in older adults.
Exploring these questions, and others you may have about scientific research, can help you be an informed, critical consumer and can help you make better decisions about your own health. For more information about being an informed consumer, check out NCCIH’s resources and take charge of your health.
Post source: medlineplus