Placental GBS DNA Linked to Higher Neonatal Unit Admissions – A recent study published in Nature Microbiology investigated the link between Group B Streptococcus (GBS) DNA in the placenta and neonatal morbidity, specifically admission to the neonatal unit (NNU).
GBS is a common cause of early-onset neonatal sepsis (EOD), a severe infection in newborns within the first week of life. About 20% of pregnant women carry GBS in their genital tract, and without intervention, around 1% of infants from these women develop EOD.
Globally, GBS is responsible for approximately 230,000 cases of EOD, contributing to roughly 50,000 stillbirths and 50,000-100,000 infant deaths. While EOD is rare in high-income countries, it is more prevalent in low-income settings.
Previous research has identified GBS as the sole bacteria in the placenta before labor in term pregnancies. Further studies are needed to understand the mechanisms by which GBS in the placenta leads to neonatal morbidity and to develop targeted interventions for prevention and treatment.
Study Design
The present study utilized data and samples from a prospective cohort of nulliparous women with a single pregnancy who received antenatal care at the Rosie Hospital in Cambridge, United Kingdom (UK), from 2008 to 2013.
The study excluded women with multiple pregnancies. Participants were recruited around 12 weeks of gestation and followed up at 20, 28, and 36 weeks of gestational age.
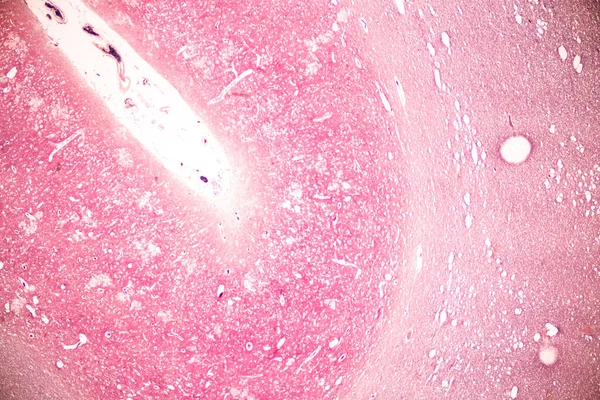
After delivery, the placenta, umbilical cord, and fetal membranes were systematically sampled, flash-frozen for molecular analysis, and fixed for microscopy. Umbilical cord blood was collected from approximately one-third of the participants.
Outcome data were collected from the mother’s medical records, electronic databases, and microbial cultures performed during the pregnancy.
A pregnancy outcome prediction (POP) study was conducted with a sample size of 4,212 women. The researchers recorded height, median age, body mass index (BMI), and interquartile ranges.
Ethical approval was obtained from the Cambridgeshire 2 Research Ethics Committee with reference number 07/H0308/163. Informed consent was obtained from all participants in written form.
Study Results
The study focused on 436 term fetuses who were admitted to the NNU within 48 hours and beyond 48 hours after delivery.
The results showed that 23.3% of term infants with placental GBS DNA and 8.4% without were admitted to the NNU. This indicates a significant association between placental GBS DNA and NNU admission, even after adjusting for maternal characteristics.
A validation study involving non-overlapped 239 cases of term NNU admissions and 686 term control groups replicated the results of the first study, confirming the link between placental GBS DNA and increased NNU admissions.
Further analysis distinguished septic from non-septic phenotypes of neonatal morbidity. The study categorized NNH admissions according to clinical proof of sepsis, from none to confirmed GBS sepsis.
Placental GBS was significantly associated with admissions into the NNU, where probable, culture-negative, and proven GBS sepsis were considered outcome measures.
Pathological findings on the fetal membranes and umbilical cord were strongly associated with placental GBS DNA in cases accompanied by chorioamnionitis and funisitis.
The study found a higher prevalence of GBS-positive placentas in participants with a positive high vaginal swab (HVS) for GBS during pregnancy compared to those with a negative HVS or no HVS culture.
The researchers found no association between the detection of GBS DNA in the placenta and the timing of births or methods of deliveries.
Additional tests to confirm the GBS DNA signal, involving novel reverse transcriptase-quantitative polymerase chain reaction (RT-qPCR) assay for GBS 16S ribosomal ribonucleic acid (rRNA), proved that these findings were reliable.
Analysis of pro-inflammatory cytokines in umbilical cord serum from term births with GBS-positive placentas revealed a ‘cytokine storm’ – a significant elevation of cytokines – compared to GBS-negative cases. This suggested an exaggerated inflammatory response to the pathogen.
Finally, the study detailed the clinical features of cases with proven and probable GBS sepsis. It found that only a minority of these cases had GBS colonization detected antenatally or received antibiotics in labor.
Implications
The study’s findings have significant implications for clinical practice, particularly concerning the screening and treating GBS in pregnant women.
Current guidelines recommend screening all pregnant women for GBS at 35-37 weeks of gestation. Those who test positive receive intrapartum antibiotic prophylaxis (IAP) to prevent neonatal GBS infection.
However, the study suggests that screening earlier in pregnancy and/or treating all pregnant women with GBS, regardless of screening results, may be more effective in reducing neonatal morbidity.
The study also highlights the need for further research to understand the mechanisms by which GBS in the placenta leads to neonatal morbidity and to develop targeted interventions for prevention and treatment.
In addition to the implications for clinical practice, the study’s findings also have important implications for public health.
GBS is a major cause of neonatal morbidity and mortality worldwide, particularly in low-income countries where access to screening and treatment is limited.
The study’s findings could inform the development of more effective GBS prevention and treatment strategies for resource-limited settings.
Future Directions
Future research should focus on the following areas:
- Develop more sensitive and specific methods for detecting GBS in the placenta
- Understand the mechanisms by which GBS in the placenta leads to neonatal morbidity
- Develop targeted interventions for the prevention and treatment of neonatal GBS infection
- Develop more effective GBS prevention and treatment strategies for resource-limited settings
The study’s findings are an important step forward in our understanding of GBS and its impact on neonatal health.
With further research, we can develop more effective strategies to prevent and treat this serious infection and improve the outcomes for newborns worldwide.
In conclusion, the presence of GBS DNA in the placenta is strongly associated with an increased risk of neonatal morbidity, evidenced by NNU admission.
This association was consistent across different analytical methods and highlighted the potential for an exaggerated inflammatory response in neonates, leading to severe outcomes.
Study source. Continue to check our website soundhealthandlastingwealth.com for more articles of this kind. And, please use our comment section as well, we would love to hear from you.