Study Explores the Link Between Microbiome And Post-Traumatic Stress Disorder Outcomes – In the aftermath of traumatic stress, individuals often experience enduring negative consequences on their psychological and physical well-being. These post-traumatic neuropsychiatric sequelae (APNS) encompass conditions like post-traumatic stress disorder (PTSD), depression, and various somatic or physical symptoms. However, the precise mechanisms underlying these adverse effects remain elusive. A recent study published in Translational Psychiatry delved into the potential role of the microbiome-gut-brain axis in mediating this association.
What Is Post-Traumatic Stress Disorder?

According to research, post-traumatic stress disorder (PTSD) is a mental health condition that some people develop after experiencing or witnessing a life-threatening event, like combat, a natural disaster, a car accident, or sexual assault. While it’s natural to feel afraid during and after a traumatic event, for people with PTSD, these feelings last much longer and can interfere with their daily lives.
Symptoms of PTSD can include:
- Reliving the traumatic event: This may happen in the form of flashbacks, nightmares, or intrusive thoughts.
- Avoiding reminders of the event: This may include avoiding places, people, or activities that remind them of the trauma.
- Negative changes in thinking and mood: This may include feeling on edge, irritable, or detached from others.
- Changes in physical and emotional reactions: This may include difficulty sleeping, feeling jumpy or startled, or having difficulty concentrating.
If you think you or someone you know may have PTSD, it’s important to seek professional help. With treatment, most people with PTSD can recover and live healthy lives.
What Is Microbiome?
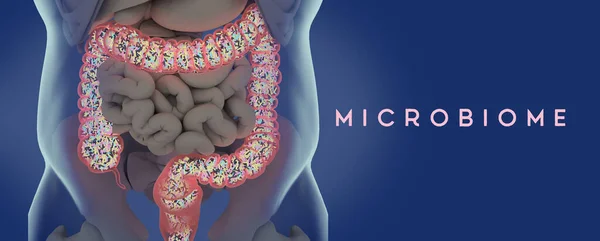
The microbiome is the community of microorganisms, such as bacteria, fungi, and viruses, that live on or in a particular organism. In humans, the microbiome is found in many parts of the body, including the skin, mouth, gut, and vagina. Microbiomes are essential for human health, and they play a role in many bodily functions, including digestion, metabolism, and immune function.
The human microbiome is made up of trillions of microorganisms, and each person has a unique microbiome. The composition of the microbiome can change over time, and it is affected by factors such as diet, environment, and medication.
A healthy microbiome is essential for human health. Microorganisms in the gut, for example, help to break down food and absorb nutrients. They also produce compounds that can help to protect against disease.
Study Background
The influence of the microbiome-gut-brain axis on brain function has been widely documented in individuals with neuropsychiatric disorders. This influence is partly attributed to the metabolites produced by gut microbes, including physiologically active chemicals and neurotransmitters. Some microbes produce short-chain fatty acids (SCFAs) like butyrate, which play a crucial role in maintaining the integrity of the gut epithelial barrier and crossing the blood-brain barrier (BBB), ultimately exerting an anti-inflammatory effect on the brain. Others, such as Enterobacteriaceae, release lipopolysaccharides (LPS), potent endotoxins that activate the Toll-like receptor (TLR) 4 pathway, triggering a surge of inflammation.
Supporting the theory that the microbiome-gut-brain axis might underlie APNS, prior research has demonstrated differences in the microbiome composition between PTSD and non-PTSD individuals, such as lower diversity and an increased abundance of opportunistic pathogens. Animal models have also shown a shift in microbial profile with stress, associated with higher levels of inflammation at both local and systemic levels.
The Study’s Findings
The study examined stool samples from 51 trauma patients enrolled in the Advancing Understanding of RecOvery afteR traumA (AURORA) study. The participants’ average age was 52 years, and the samples were collected an average of 45 days after their emergency department (ED) visit following a traumatic event. Over 60% were White, mostly non-Hispanic, and a quarter were Black.
The participants were evaluated for post-traumatic stress disorder (PTSD), depression, and somatic symptoms using standardized assessment tools. These evaluations were then analyzed to reveal associations between demographic features, microbial profile, and APNS. Both microbial abundances and microbial metagenomics were considered in this analysis.
The results revealed that the gut microbiome profile explained about half the variation in PTSD, a quarter in depression, and 44% in somatic symptoms. For PTSD, three microbes showed a linear increase in abundance with symptom severity, while one of them was also correlated with increasing depression severity. Two other species were enriched in association with somatic symptom severity.
Additionally, the researchers identified important highly prevalent commensal microbial species like Flavonifractor plautii, Ruminococcus gnavus, and Bifidobacterium species as predictors of APNS outcomes, depending on the abundance data. B. adolescentis, B. longum, and Flavonifractor plautii were among the top five predictors for all three APNS outcomes.
Conversely, metagenomics data revealed shifts in the amino acid biosynthetic pathways with all three APNS outcomes. In humans, L-ornithine can be synthesized de novo or converted to arginine, making the L-arginine, ornithine, and citrulline pathways interconvertible. The citrulline biosynthesis pathway was inversely associated with poorer outcomes in all three areas. Meanwhile, L-arginine and polyamine biosynthesis was the best predictor of PTSD and third among depression predictors, varying negatively with PTSD and depression scores.
The bacterium E. coli participated at a higher level in all arginine-ornithine biosynthetic pathways but produced a smaller fraction of the total L-citrulline in people with PTSD vs more in those with depression. Conversely, Ruminococcus contributed less to L-arginine production through both pathways. Other microbes from the genera Flavonifractor and Faecalibacterium were more active in converting ornithine to L-arginine in people with PTSD or depression.
Implications
The study’s findings suggest that individuals with higher abundances of certain commonly occurring microbial species are more likely to develop APNS. Demonstrated differences in microbial abundances accounted for one-fifth to one-half of the observed variations in APNS outcomes, comparable to that attributed to clinical and demographic profile differences.
The models identified two significant predictors for all APNS outcomes: Bifidobacterium species and Flavonifractor plautii. Despite not fully corroborating all previous studies, this emphasizes the need to develop more comprehensive microbiome models when assessing potential associations beyond the species level.
The association of APNS with microbiome changes might be mediated by lower arginine availability for the body due to gut microbiome activity, reflecting a metabolic shift also observed in plasma samples from PTSD patients. This is evident in the altered contributions to pathways for the biosynthesis of the linked amino acids arginine, citrulline, and ornithine.
The global arginine bioavailability ratio (GABR) is measured as the ratio of arginine to ornithine and citrulline, its breakdown products. Changes in arginine metabolism could alter arginine vasopressin or nitric oxide (NO) levels, affecting multiple neuropsychiatric pathways. Further research will be needed to identify how exactly different microbial species contribute to these shifts.
In conclusion, the study provides convincing evidence of a link between the gut microbiome and APNS outcomes, potentially mediated by microbial metabolites and shifts in amino acid biosynthesis pathways.
Resources:
- Translational Psychiatry: https://www.nature.com/articles/s41398-023-02643-8
- National Center for PTSD: https://www.ptsd.va.gov/: https://www.ptsd.va.gov/
- The Trauma Survivors Network: http://traumasurvivorsnetwork.org/
- The Rape, Abuse & Incest National Network (RAINN): https://www.rainn.org/
Continue to check our website for more articles of this kind. And, please use our comment section as well, we would love to hear from you.