Coronavirus is a family of viruses that cause diseases in birds and mammals, including humans. Common cold, Middle East Respiratory Syndrome (MERS-CoV) and Severe Acute Respiratory Syndrome (SARS-CoV) are examples of diseases caused by Coronaviruses. Symptoms and signs can be mild but may become severe and deadly if care is not taken.
Coronaviruses have existed for decades but have become a subject of global discussion since the year 2019 (December) after when it broke in Wuhan China.
Medical researchers believe that the 2019 Coronavirus disease (COVID-19) outbreak that started in Wuhan china before crossing over to other countries was caused by a new virus called severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2).
In the bid to control the COVID-19 illness from spreading further, the World Health Organization (WHO) and the U.S. Centers for Disease Control and Prevention (CDC) came up with treatment and preventive guidelines. In recent times, we have vaccines and treatment options that are effective in reducing the risk of severe illness, hospitalization, and death from COVID-19.
The updated bivalent COVID-19 vaccines, designed to target the Omicron variant and original strain, are recommended for everyone eligible according to the CDC’s Advisory Committee on Immunization Practices.
Causes of coronavirus
SARS-CoV-2 Virus: COVID-19 is caused by infection with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a novel coronavirus that emerged in late 2019. It spreads primarily through respiratory transmission and can mutate to produce new variants that may impact the effectiveness of treatments and preventive measures over time.
In simple term, what causes coronavirus in humans is when a healthy living person makes close contact with a coronavirus carrier individual or animal. In 2019, Scientists at the Chinese Center for Disease Control and Prevention said tests showed that humans acquired COVID-19 from animals at the Wuhan animal market where live animals were being traded. Even though some experts believe the disease originated from snakes as they are known carriers of coronaviruses. Coronaviruses are zoonotic, meaning animals are the primary hosts of these viruses before transmitting to humans.
Researchers believe SARS was transmitted from bats to civet cats and then to humans. While MERS moved from camels to humans.
COVID-19 transmission: Understanding the modes of spread
Coronavirus can spread through person-to-person contact says “China’s National Health Commission“. Understanding how the virus transmits from person to person is crucial for implementing effective prevention measures. Here’s how the transmission happens;
Respiratory Droplets is one of the primary transmission routes. When an infected person coughs, sneezes, talks or breathes, they release respiratory droplets containing the virus. These droplets can directly infect others who are in close contact (within 6 feet) by entering their nose, mouth or eyes
Airborne Transmission: In some situations, such as during medical procedures that generate aerosols, the virus can remain suspended in the air in smaller particles called aerosols. These can be inhaled by others, leading to infection at distances greater than 6 feet.
Surface (Fomite) Transmission: The virus can contaminate surfaces and objects that an infected person has coughed, sneezed or touched. Others can then pick up the virus by touching these surfaces and then touching their own face, nose, mouth or eyes.
Fecal-Oral Transmission: JAMA Network and PlOS ONE Studies have detected the virus in the stool of infected individuals, suggesting a potential fecal-oral route of transmission, though this has not been definitively proven.
Mother-to-Child Transmission: According to World Health Organization, vertical transmission from an infected mother to her child during pregnancy, childbirth or breastfeeding is possible but appears to be rare.
COVID-19 symptoms: Onset timing varies across Infected Individuals
The Centers for Disease Control and Prevention (CDC) reports that typical COVID-19 symptoms often appear 2 to 14 days after exposure to the SARS-CoV-2 virus. In some cases, symptoms resembling a common cold can manifest as early as 2 days after infection. However, in other cases, it may take up to 14 days before any symptoms become visible.
International Journal of Environmental Research and Public Health report published in 2022 revealed that the estimated median incubation period for the Omicron variant was 2.8 days, significantly shorter than the 4.5 days observed for the Alpha variant and the 3.7 days estimated for the Delta variant. This suggests that the timing of symptom onset can vary depending on the specific SARS-CoV-2 variant causing the infection.
It is important to note that some infected individuals may remain asymptomatic throughout the course of their infection, while others may develop severe symptoms requiring hospitalization. Factors such as age, underlying health conditions, and vaccination status can also influence the timing and severity of COVID-19 symptoms.
Symptoms of COVID-19 include…
- fever
- cough
- runny nose
- sore throat
- headache
- sneezing
- fatigue
- shortness of breath or breathing difficulty
In more severe cases, coronavirus infection may cause people with premature or weak immune systems, children and infants, old adults, people with heart or lung disease to have…
- pneumonia
- diarrhea
- severe acute respiratory syndrome,
- kidney failure,
Note: All these symptoms should not be taken as minor as they may even lead to death.
Risk factors
- Being a male
- People who smoke
- People with a sedentary lifestyle
- Unvaccinated individuals
- Infants and children with a premature immune system are most likely to be infected.
- Older people with low-performing immune systems.
- School children such as those in daycare, boarding homes, or colleges.
- People who have a weak immune system
- Adults or children with certain medical conditions such as diabetes and heart disease, chronic kidney disease, chronic obstructive pulmonary disease (COPD), cancer, HIV and HIV, transplant medications
- Those using certain medications including chemotherapy drugs
- Tourists and travellers especially those who reside or travel to China and other high-risk countries with coronavirus cases.
- Those who worship in various religious centers.
- Those who keep close contact with coronavirus-infected persons.
When to seek medical help
If you have any of the coronavirus symptoms mentioned or you feel exposed to the virus, contact your doctor immediately. Over the phone, tell your doctor about your recent association with people, where you have been to and things you got exposed to. Make sure your doctor confirms your appointment before the visit.
Additionally, consult your doctor if you have a very high fever (over 40°C/104°F) that persists for more than 3 days, or if you experience symptoms like severe headache, uncontrollable shivering, or unusual drowsiness, chronic cough, breathing changes, dehydration, unusual tiredness, confusion, dizziness, lack of urination, or a weak/rapid pulse.
Some people with COVID-19 may require hospitalization and treatments like oxygen therapy, COVID-19 medications, or mechanical ventilation if their condition becomes severe.
The goal is to closely monitor your symptoms and seek prompt medical attention if you experience any concerning or worsening signs, especially if you are at higher risk for severe illness. Acting quickly can be crucial for managing COVID-19 effectively.
Diagnosis
In a simple term, Just like other viral infections, the 2019 coronavirus disease can be diagnosed with samples of blood, saliva, or tissue drawn from a person. A laboratory technician will either draw a sample of your blood with a needle or use a cotton swab to take from your nose or back of your throat a small sample of saliva or respiratory secretions. These samples will then be used to run laboratory tests such as serology tests and molecular tests so as to detect the infection or the type of virus a person has been exposed to.
Put differently in a more medical term, according to the Journal of Clinical Laboratory Analysis, coronavirus infections, including COVID-19, are primarily diagnosed through the following methods:
Molecular tests: These tests detect the genetic material (RNA) of the SARS-CoV-2 virus that causes COVID-19. The most common molecular test is the reverse transcription polymerase chain reaction (RT-PCR) test, which is considered the gold standard for COVID-19 diagnosis. RT-PCR tests involve collecting a sample, usually from the nose or throat, and then using laboratory equipment to amplify and detect the viral RNA.
Other molecular tests include isothermal nucleic acid amplification tests and CRISPR-based tests, which can provide faster results than RT-PCR. These tests also detect the presence of SARS-CoV-2 genetic material.
Antigen tests: These tests detect specific proteins on the surface of the SARS-CoV-2 virus. Antigen tests are faster and cheaper than molecular tests, but generally less sensitive. Antigen tests are useful for rapid screening, especially in symptomatic individuals.
Antibody tests: These tests detect antibodies produced by the immune system in response to a SARS-CoV-2 infection. Antibody tests can indicate a past infection but are not recommended for diagnosing an active, current infection.
Imaging tests: Chest X-rays and CT scans can sometimes show lung abnormalities associated with COVID-19, but these are not definitive diagnostic tests.
Treatment options for coronavirus Infections
The good news is that there have been significant advancements in treatment options for COVID-19 since the initial outbreak. Here are the treatment options currently available.
Antiviral medications: Remdesivir (brand name Veklury) is the first FDA-approved antiviral drug for the treatment of COVID-19. It is used to treat hospitalized patients aged 12 and older. Other antiviral medications, such as:
Paxlovid (nirmatrelvir and ritonavir) an FDA-approved oral medication highly effective against COVID-19 if started within 5-7 days of symptoms. Lagevrio (molnupiravir), is another oral option, Lagevrio has also been shown to be effective for mild to moderate cases.
Over-the-counter medications like acetaminophen or ibuprofen can also help manage fever and aches. Rest and plenty of fluids are crucial for recovery.
Immune modulators: Clinical trials are studying the use of immune modulators, which can help minimize the effects of an overactive immune system response in some COVID-19 patients. These treatments aim to reduce the need for ventilators and shorten hospital stays.
Antibody treatments: Monoclonal and polyclonal antibody therapies are being tested in both inpatient and outpatient settings to determine if they can shorten recovery time and lessen respiratory and other complications from COVID-19 infection.
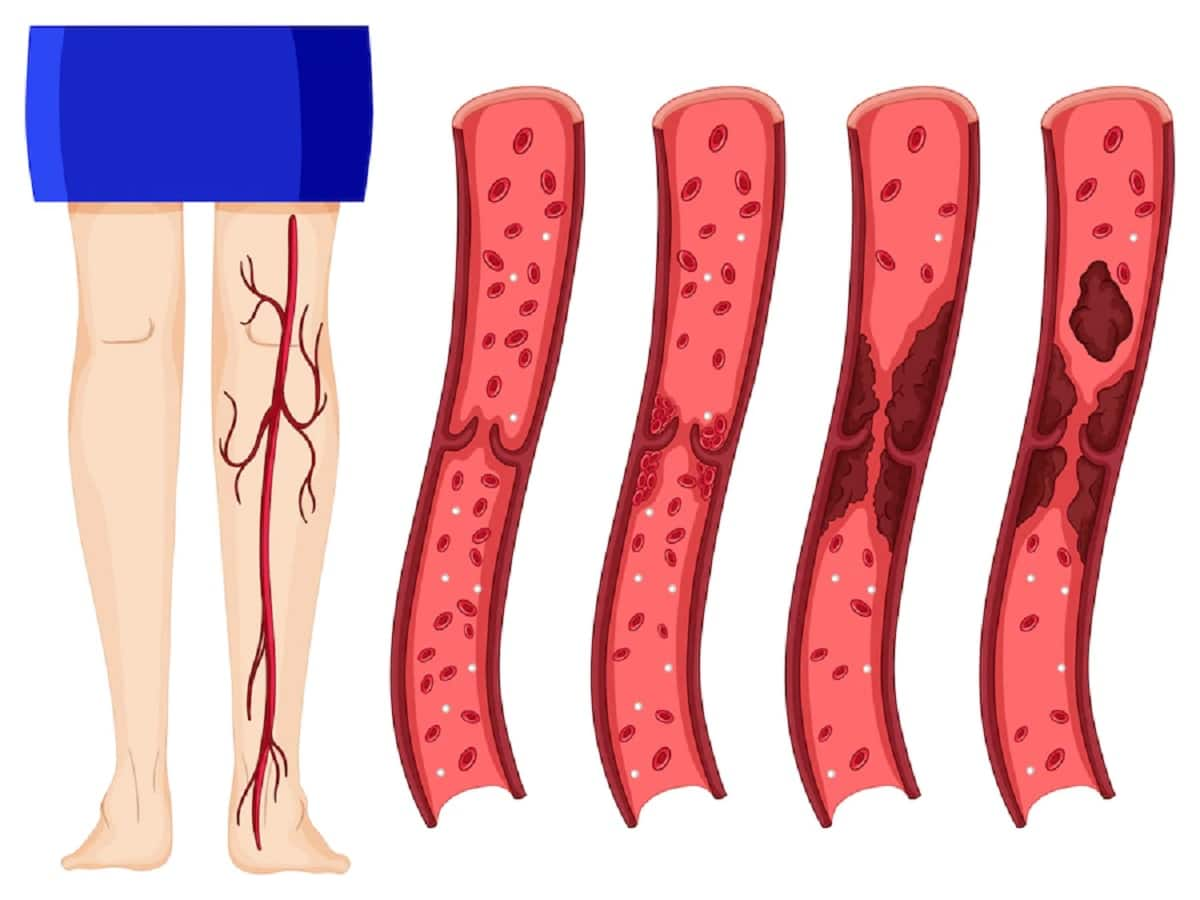
Blood thinners: Studies are evaluating whether blood thinners can help treat COVID-19-associated coagulopathy (blood clotting disorders) and prevent life-threatening blood clots in hospitalized patients.
Supportive care: For more severe cases, hospitalized patients may receive supplemental oxygen, fluids to prevent dehydration, fever-reducing medications, and ventilator support if needed.
For Severe Illness (Hospitalized Patients):
- Remdesivir: This intravenous antiviral medication can help shorten hospital stays for some patients, especially when combined with corticosteroids.
- Corticosteroids (e.g., dexamethasone): These medications can help reduce inflammation caused by the overactive immune response in severe cases.
- Other Immunomodulatory Therapies: Newer therapies like baricitinib and tocilizumab may be used in certain cases to regulate the immune system’s response to the virus.
- Convalescent Plasma: In some situations, plasma from recovered COVID-19 patients may be used for patients with weakened immune systems who don’t respond well to other treatments.
- Supportive Care: Oxygen therapy, mechanical ventilation (if needed), and other critical care interventions are essential for severely ill patients.
Prevention – How to prevent coronavirus Infection (COVID-19)
According to WHO and CDC recommendations, the most effective ways to prevent coronavirus infection (COVID-19) are:
Vaccination: Getting vaccinated is the primary defense against COVID-19. The updated bivalent vaccines, designed to target the Omicron variant and original strain, have been shown to significantly lower the risk of severe illness, hospitalization, and death from COVID-19, even against newer variants like FLiRT.[1,5] Everyone eligible should stay up to date with the recommended COVID-19 vaccine doses.
Masking: Universal masking, especially in healthcare settings, has been proven to prevent most SARS-CoV-2 transmissions. Wearing a well-fitted mask in crowded indoor spaces or when physical distancing is difficult can reduce the spread of COVID-19.
Ventilation: Ensuring adequate ventilation, with at least five clean air changes per hour, is an important measure to prevent COVID-19 transmission in indoor settings like hospitals. Opening windows, using HEPA filters, and improving airflow can reduce the concentration of virus particles in the air.
Testing and Isolation: Regular testing of healthcare workers and patients, regardless of symptoms, combined with strict isolation protocols for those infected, has been effective in limiting the spread of COVID-19 in healthcare facilities. Staying home and maintaining social distancing or isolating when sick or after a known exposure can prevent passing the virus to others.
Handwashing and Hygiene: Practicing good hand hygiene by frequently washing with soap and water for at least 20 seconds, or using 60% alcohol-based hand sanitizer, covering coughs and sneezes with your elbow, towel, or tissue, and avoiding touching the face can help stop the transmission of COVID-19 through contaminated surfaces or droplets.
While COVID-19 continues to evolve, these prevention strategies, used in combination, remain the most effective ways to protect individuals and communities from infection.
More Preventive Options
- Do not touch your nose, eyes, and mouth with unclean hands.
- Avoid contact with live animals around your living area, markets or places that have recently had new coronavirus cases.
- Avoid close contact with sick people.
- Get quality rest always.
- Drink plenty of water every day.
- Stay away from crowded gatherings and events
- Personalize your items. Avoid sharing dishes, glasses, bedding and other household items with people especially those who are sick.
- Clean and disinfect hard surfaces that you frequently touch.
- Do not go to work or public areas if you feel sick and speak to your doctor immediately.
- Avoid eating raw or undercooked meat or animal organs.
- Take medications as soon as you notice symptoms and don’t let the condition get severe.
In addition, boosting your immune system can help you stay protected and even fight off the virus from your body if you have it.
Extra Resources
- https://iris.who.int/bitstream/handle/10665/339422/WHO-2019-nCoV-mother-to-child-transmission-2021.1-eng.pdf?sequence=1
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8761393/
- https://www.spandidos-publications.com/10.3892/ijmm.2021.4933
- https://www.mdpi.com/2072-666X/13/8/1349
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8409760/
- https://covid19.nih.gov/covid-19-treatments
- https://www.healthline.com/health/coronavirus-treatment
- https://www.cdc.gov/coronavirus/2019-ncov/your-health/treatments-for-severe-illness.html
- https://www.mayoclinic.org/diseases-conditions/coronavirus/diagnosis-treatment/drc-20479976
- https://aspr.hhs.gov/COVID-19/Therapeutics/Pages/default.aspx
- https://www.cdc.gov/coronavirus/about/prevention.html
- https://www.covid19treatmentguidelines.nih.gov/overview/prevention-of-sars-cov-2/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3127101/
More about: |Diseases